Imagine Sarah, a vibrant woman in her late 30s, who used to hike mountains every weekend. Then came COVID, and even after the acute infection passed, a relentless fatigue clung to her, accompanied by muscle pain and brain fog. She visited doctor after doctor, only to be met with skepticism. “It’s probably stress,” one said. “Just anxiety,” another dismissed. Sarah’s story, unfortunately, is not unique; it’s a common narrative illustrating the profound invisible disability healthcare gaps in the USA. However, a growing number of patients are finally finding relief at specialized clinics in the USA dedicated to complex chronic conditions.
Why are Invisible Disabilities like Long COVID or Fibromyalgia Often Dismissed by US Doctors?
The dismissal Sarah experienced is a harsh reality for many with conditions like Long COVID, fibromyalgia, and chronic fatigue syndrome (ME/CFS). These illnesses, often lacking clear biomarkers or visible signs, frequently fall into a diagnostic blind spot within conventional medicine. Many US doctors are trained to identify acute, observable conditions, not complex, multi-system chronic illnesses.
This leads to frustrating cycles where patients are told their symptoms are “all in their head,” delaying effective Long COVID treatment USA and exacerbating patient suffering. The critical role of specialized clinics in the USA is to counter this diagnostic uncertainty with expert, integrated care. The lack of comprehensive medical education on these conditions contributes significantly to this problem, creating substantial healthcare gaps chronic illness patients face.
Why do Women with Fibromyalgia Face Healthcare Bias in the US?
Gender bias undeniably plays a role in the dismissal of invisible disabilities, particularly for women. Historically, conditions like fibromyalgia were often labeled as “hysteria” or psychosomatic. Studies, such as those from the National Institutes of Health, acknowledge that women are disproportionately affected by chronic pain conditions and frequently report their pain being taken less seriously than men’s. This systemic bias means that women, often the majority of patients seeking help for conditions like fibromyalgia, encounter an uphill battle to be believed and receive appropriate care. Access to specialized fibromyalgia clinics in the US becomes even more critical for this demographic.

What Healthcare Gaps Exist for Chronic Fatigue Syndrome in the US?
For those battling chronic fatigue syndrome (ME/CFS), the healthcare gaps chronic illness are particularly pronounced. Despite being recognized by the CDC as a serious, long-term illness, ME/CFS often lacks dedicated resources and knowledgeable practitioners. Patients struggle with fragmented care, jumping from specialist to specialist, none of whom truly understand the intricate nature of the condition. There’s a severe shortage of research funding compared to other chronic illnesses, further limiting diagnostic tools and effective chronic fatigue care strategies. This often leaves individuals feeling isolated and without a clear path to recovery.
How Can Specialized Clinics Support Patients with Invisible Conditions?
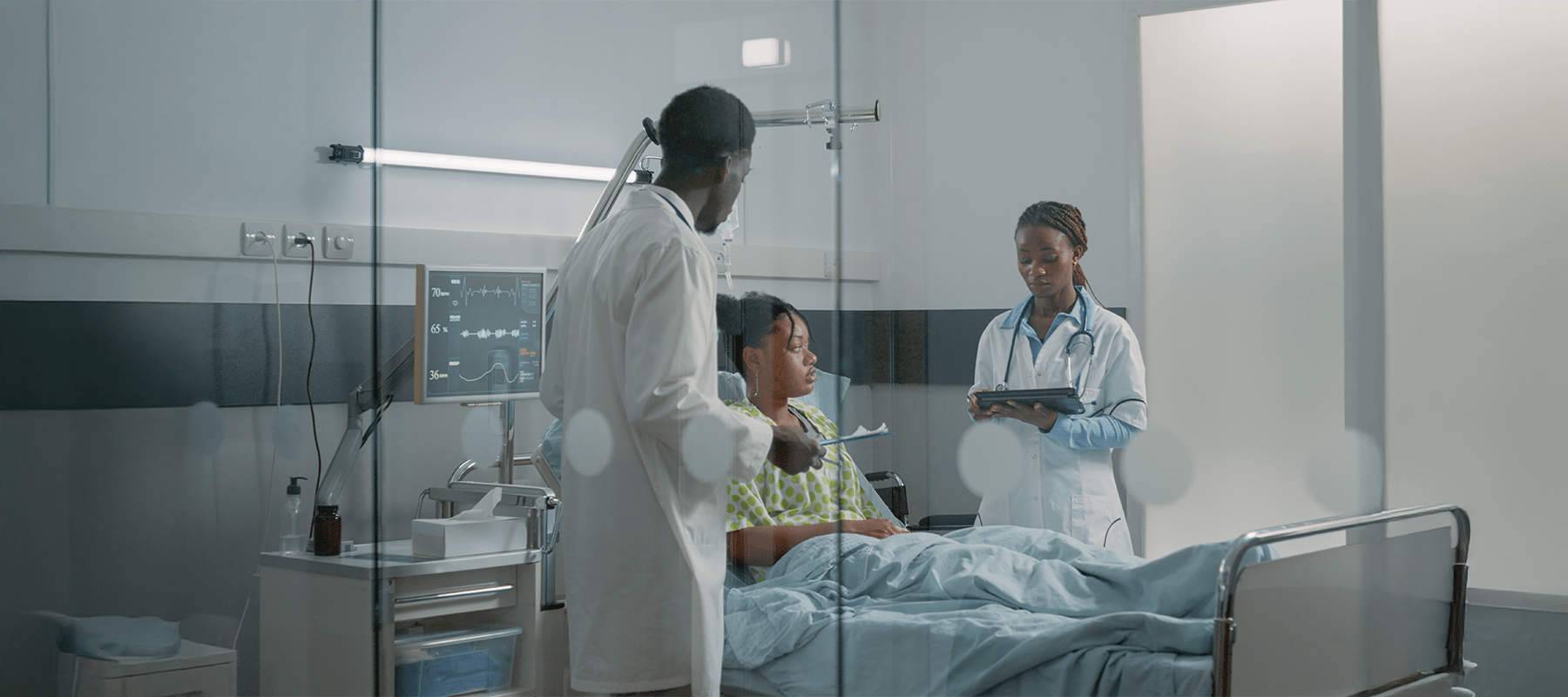
The solution, or at least a significant part of it, lies in the rise of specialized clinics in the USA. These centers offer a lifeline to patients like Sarah. They bring together a multidisciplinary team – neurologists, rheumatologists, pain specialists, physical therapists, and mental health professionals – all under one roof, with a shared understanding of complex invisible illnesses. Their approach is holistic, acknowledging the interconnectedness of physical and mental health, and they are often at the forefront of implementing new diagnostic and treatment protocols for Long COVID treatment USA and similar conditions.
What Challenges do Americans with Invisible Disabilities Face in Getting Proper Diagnosis and Care?
Beyond dismissal and bias, Americans with invisible disabilities navigate a labyrinth of challenges: insurance hurdles for non-standard treatments, long wait times for expert opinions, and the sheer emotional toll of constantly advocating for their own health. The lack of coordinated invisible disability healthcare means patients spend countless hours researching, coordinating appointments, and battling for recognition. This journey is exhausting and often leads to a worsening of symptoms due to delayed or inadequate chronic fatigue care.

Redemption Through Specialized Care: A Glimmer of Hope
Sarah eventually found a specialized clinic focusing on post-viral syndromes. Her new doctor listened intently, validating her experiences. She received a comprehensive evaluation, leading to a diagnosis of Long COVID and a personalized treatment plan incorporating gentle physical therapy, nutritional guidance, and cognitive behavioral therapy to manage her brain fog. It wasn’t an overnight cure, but it was hope.
The clinic’s integrated approach transformed her outlook and significantly improved her quality of life. My personal viewpoint is that these specialized clinics in the USA are not just treatment centers; they are sanctuaries of understanding and validation for those previously overlooked. They are a critical step in bridging the immense healthcare gaps chronic illness patients endure.
What Policy or Healthcare Changes Could Improve Care for Patients with Invisible Disabilities?
Improving care requires systemic changes: increased funding for research into invisible illnesses, mandatory medical education on conditions like ME/CFS and fibromyalgia, and policy reforms that incentivize the development and accessibility of specialized clinics in the USA. Furthermore, promoting diagnostic criteria that account for the subjective experience of invisible illness, rather than solely relying on objective markers, is crucial. This will help ensure that invisible disability healthcare moves towards a truly patient-centered model.
Conclusion
The struggle of Sarah and millions of Americans with invisible disabilities is a clear indictment of the deep-seated healthcare gaps chronic illness patients face. The dismissal of conditions like Long COVID, fibromyalgia, and ME/CFS stems from systemic issues: lack of research, physician bias, and a diagnostic framework that prioritizes the visible. However, the emergence and proliferation of specialized clinics in the USA offer a tangible path toward redemption.
These integrated centers provide the expert validation and comprehensive invisible disability healthcare that traditional systems often deny. To truly improve the lives of these patients, the US healthcare system must move beyond skepticism and actively invest in expanding these specialized care models, ensuring that every American battling an unseen illness can access the coordinated, evidence-based Long COVID treatment USA and chronic fatigue care they deserve. The time for dismissing the invisible is over; the time for integrated solutions is now.

Pamela is a creative content writer and editor with experience working with various multinational agencies. She is known for her dynamic approach and enthusiasm in publishing engaging and insightful articles.