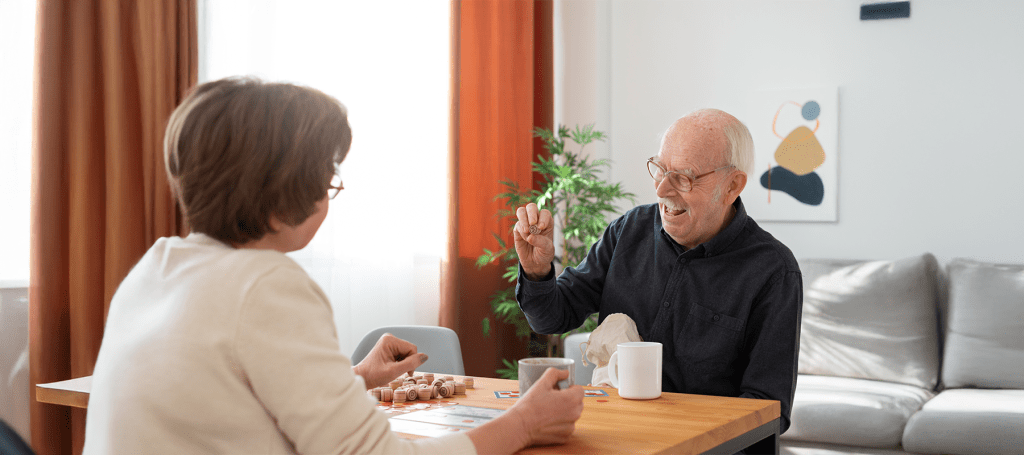
How can I forget my mother! Once a sharp, witty, and independent soul, she suddenly seemed so lost behind a fog of confusion. The moment when her soft, trembling hands clutched mine in her nursing home room will remain etched in my mind forever. But her quick personality change after new medications started actually confused me the most. This is the very moment that fuelled my investigation into a growing crisis – overmedication of seniors in nursing homes, and even why antipsychotics in seniors is an emerging epidemic within America’s long-term care system.
The main causes of overmedication of seniors in nursing homes in the USA
Overmedication of seniors in nursing homes is a deeply rooted issue powered by the complex incentives and systematic neglect. Medication management seems a lot more complicated because many US residents are suffering from multiple chronic diseases. Yet often, keeping careful assessment aside, the nursing homes are more quick to rely on drugs for behavior and distress management. There are facilities with limited medical staff and overwhelming workloads, so the convenient option is substituting attentive human care with pills.
There is also another major contributor – psychotropic drug misuse. Psychotropic drugs are often misused when the facilities are trying to control agitation or confusion in dementia patients. While these drugs temporarily work to “calm” the seniors, they cost alertness, independence, and worst of all, sometimes life itself.
Why are antipsychotic drugs still being misused as chemical restraints?
Antipsychotic usage in seniors has shifted from medical necessity to behavioral control in most facilities in the USA. Though the patients with schizophrenia or severe psychosis benefit from these drugs, they are often prescribed off-label for restlessness management and aggression control in dementia patients.
But the reality is, this practice is like the chemical restraints – residents are being sedated so they can be easily managed, but their well-being is not being catered to. According to a 2024 federal study, nearly one in five nursing homes in the USA have residents who receive antipsychotic medication, regardless of the clinical diagnosis supporting their use being available.
How did the Federal Regulations fail to stop nursing home overmedication practices?
The federal rules, like the CMS initiatives for reducing the unnecessary antipsychotic use of antipsychotics, were meant for reducing psychotropic drug misuse. Nevertheless, the enforcement remains spotty. The reason is that the facilities are involved in self-reporting data, and diagnostic loopholes are often exploited.
Moreover, the regulations have failed to fully address the deeper cause – staffing shortages that push the care providers towards chemical quick fixes, rather than compassionate caregiving.
How can the nursing home staffing shortages contribute to the overuse of psychotropic drugs?
Inadequate staffing is the major reason behind this issue. There are several nursing homes in the USA operating with minimal nurse-to-patient ratios. It is not possible for the overworked caregivers to provide the hands-on attention needed for high-need residents.
As I have seen, in my mother’s facility, one nurse was given the responsibility of caring for nearly 20 residents during each night shift. It’s fine to predict that many residents were more sedated to be easily supported. However, over time, I realized that psychotropic drug misuse cannot always be said to be intentional cruelty, but more often due to overwhelmed staff under pressure, trying to maintain control in certain unsafe conditions.
The ethical and legal implications of chemical restraints in long-term care homes
Both ethical and legal red flags are raised due to the use of chemical restraints. The practice violates the fundamental dignity and autonomy of elderly patients. In legal terms, overmedication without informed consent is equal to elder abuse, as stated by U.S. law.
Often, the families fail to realize that consent is necessary for the use of any antipsychotics in seniors. There are several cases in which they are unaware that these drugs are even being administered until the seniors experience side effects like excessive drowsiness or falls in the worst cases.
Elder care reform has to focus on transparency and accountability, more than punishment.
What are the roles the families are responsible for in preventing overmedication of elderly relatives?
Families will be able to make an enormous difference. First, the members have to learn about medications, ask direct questions, and request medication reviews. I remember clearly that I had requested a full medical audit for my mother, and was in awe when I learned she was on three unnecessary antipsychotics. Hence, I wasted no time on supervised withdrawal and enhanced engagement therapy. What made me happy was when her lucidity returned and she laughed kindheartedly.
From this experience, I have learned that awareness is the first step to prevention. Families have to be the vocal advocates against the overmedication of seniors by nursing homes.

How is the US Government addressing antipsychotic misuse in nursing homes?
Together with the Centers for Medicare & Medicaid Services, the U.S. Department of Health and Human Services has launched initiatives to track and publicly report antipsychotic use among long-term care facilities. The prime focus of new metrics is on transparency and accountability.
The recent elder care reform proposals have included financial penalties for facilities showing a high rate of psychotropic drug misuse without any clear justification.
The most effective policy reforms in protecting seniors from chemical restraints
The noteworthy and promising reforms involve multidisciplinary approaches that combine staff education, stronger oversight, and better mental healthcare. The programs meant for increasing staffing levels and offering non-drug behavioral interventions have reported declines in antipsychotic usage by nearly 25%.
The elder care reform should compulsorily prioritize humane caregiving that ensures compassion, and not chemical restraints. These are the cornerstones of long-term care.
The latest statistics on antipsychotic overprescription rates in the USA nursing homes
As per the National Partnership to Improve Dementia Care, as of 2025, about 18% of long-term care residents are continuing to receive antipsychotics in seniors without medical necessity. Even if the data is down from 25% a decade ago, the pace of improvement seems to have slowed. Psychotropic drug misuse continues to be a major concern – it signals that reform efforts are in dire need of renewed vigor.
On a final note,
My mother’s slow recovery brought out a revelation – the problem is more than medication misuse – the concern is the failing system equating silence with care. The true elder care reform calls for a shift towards empathy-driven care models, accountability, transparent reporting, and community vigilance. The road ahead invites the families, the healthcare workers, and the policymakers to work together to help the seniors from being left silenced behind chemical restraints again.

Sheila is a creative content writer and publisher of The Smile Story. With experience working with various multispecialty clinics and hospitals, she is dynamic in providing health-related guest posting services, offering insightful and impactful content.