A big city is always well-equipped with healthcare facilities – when in need, an emergency room is just a short drive away. However, in small towns, life is not the same for millions of Americans. Due to rural hospital closures across the nation, safety nets on which the families have depended for generations have begun to dismantle quietly.
So, what is the outcome to healthcare access in rural areas? Not just by numbers, but by heartbreaking delays in care, a rural healthcare crisis explained the increased risks and enlarging inequalities.
The hidden epidemic of rural ER closures has reshaped survival mode in small-town America during medical emergencies. Nevertheless, at the same time, creative solutions are sparking from telehealth to mobile clinic solutions for rural healthcare.
In this blog post, we shall gradually uphold what is happening, who is being most affected, and how the communities are fighting back.
The reason behind so many ER closures
Shrinking hospital budgets, declining patient count, and increasing costs of specialized staff are the real causes of ER shutdowns in small towns. Often, the rural hospitals are operating on razor-thin margins. Hospital boards are forced to make devastating decisions during crises, such as insurance reimbursement falling short and impossible recruitment options. Ultimately, in a strained system, rural hospital closures are much less about choice and more about survival.
How are rural hospital closures affecting everyday care?
The effects of rural ER closures are not limited to emergencies. Try to answer a question. Is it possible to drive an extra 45 minutes if anyone has encountered a stroke or has just been in a car accident? Critical response times are stretched, which narrows the minutes between life and death. In this way, if the rural healthcare crisis is explained, it is characterized by deeply personal, slower care, higher costs, and fewer options for follow-up treatment.
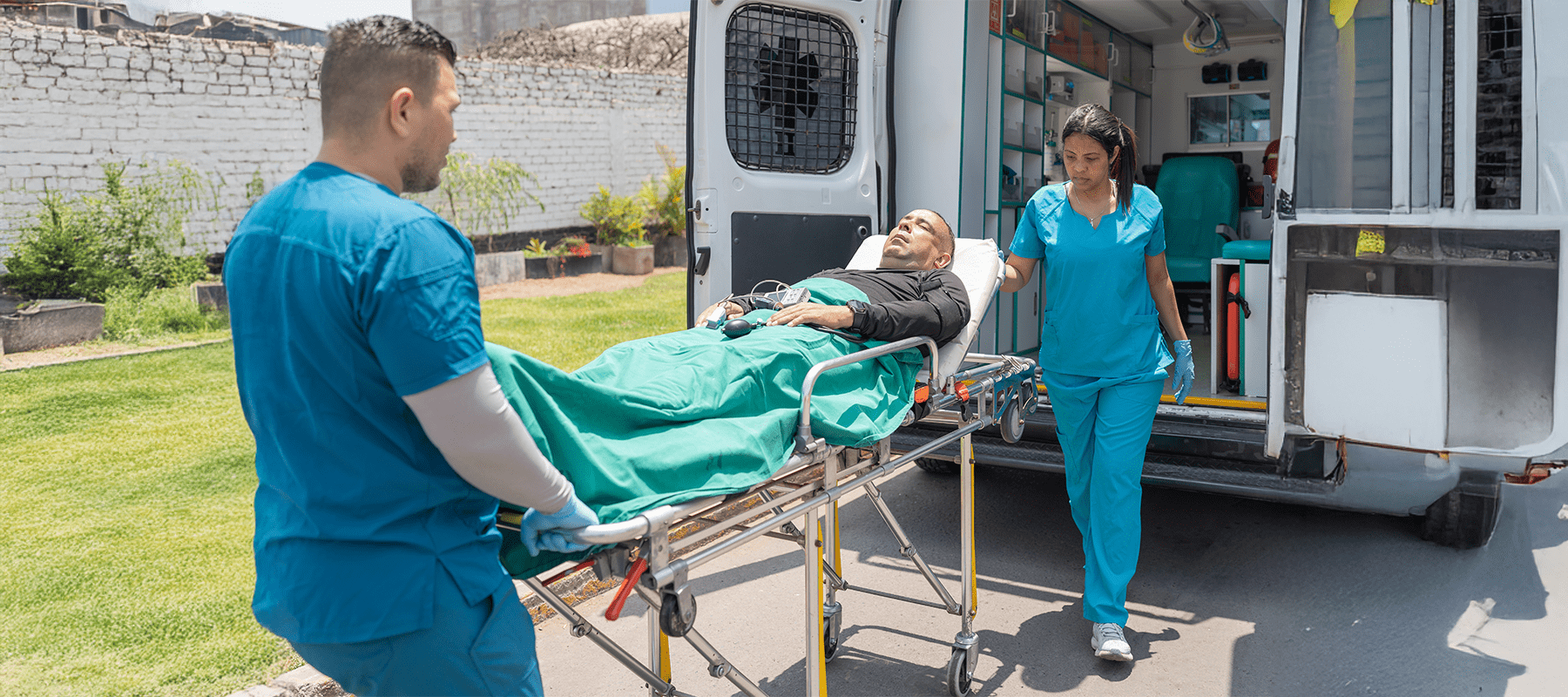
Critical care delays – a tough race against time
Ambulances have to travel longer distances when the nearest ER shuts down. In regional hospitals, the wait times spike. It is a direct influence on rural hospital closures and mortality rates. As per the notes shared by researchers, the trauma victims, expectant mothers and cardiac patients are significantly at higher risks. The truth is always stark – delays kill, and closures add to those delays.
Who are the prominent suffering individuals?
There are certain groups to whom the weight of closures feels heavier:
i. Older adults
In the rural elderly, healthcare challenges after ER closures – delayed stroke care, limited transportation options and unmanaged chronic illnesses are included.
ii. Conceiving women
The impact of hospital shutdowns on pregnant women in rural areas has triggered maternity care deserts. As a result, many pregnant women are forced to travel for hours to receive prenatal or delivery care.
iii. Children
Rural child healthcare access without ER is a real-time challenge. Children start
lacking timely pediatric emergencies and specialized care.
These groups specify that the healthcare disparities in rural communities are widening. The mobile clinic solutions are now striving to close the solutions.
The economic pressures behind the crisis
Economic fragility is also a central factor, alongside patient health and well-being. The causes of ER shutdowns in small towns are heightened mainly due to staffing shortages, burnouts and limited federal funding. Unless there is adequate reimbursement and workforce support, hospitals start closing departments. Ultimately, the entire facilities are closed down. Due to the domino effect, the result is rural hospital closures rippling through communities, threatening jobs and livelihoods, as well as health outcomes.
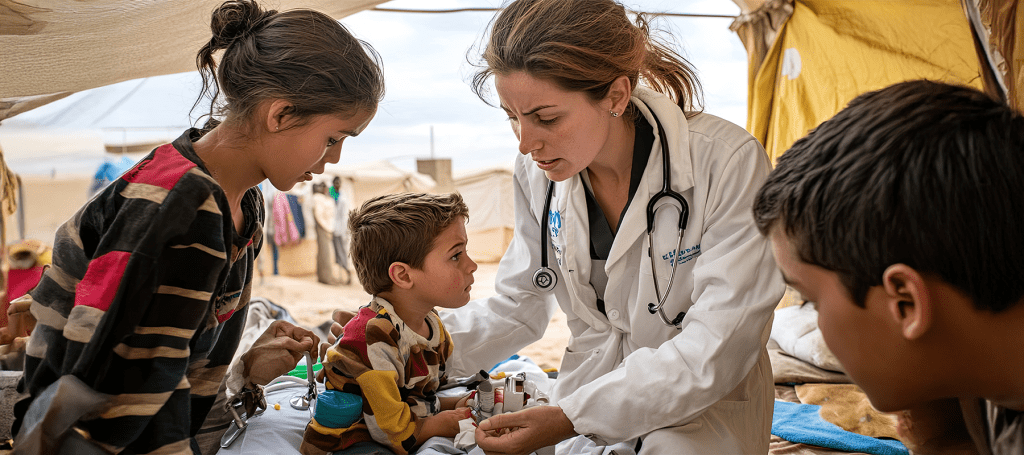
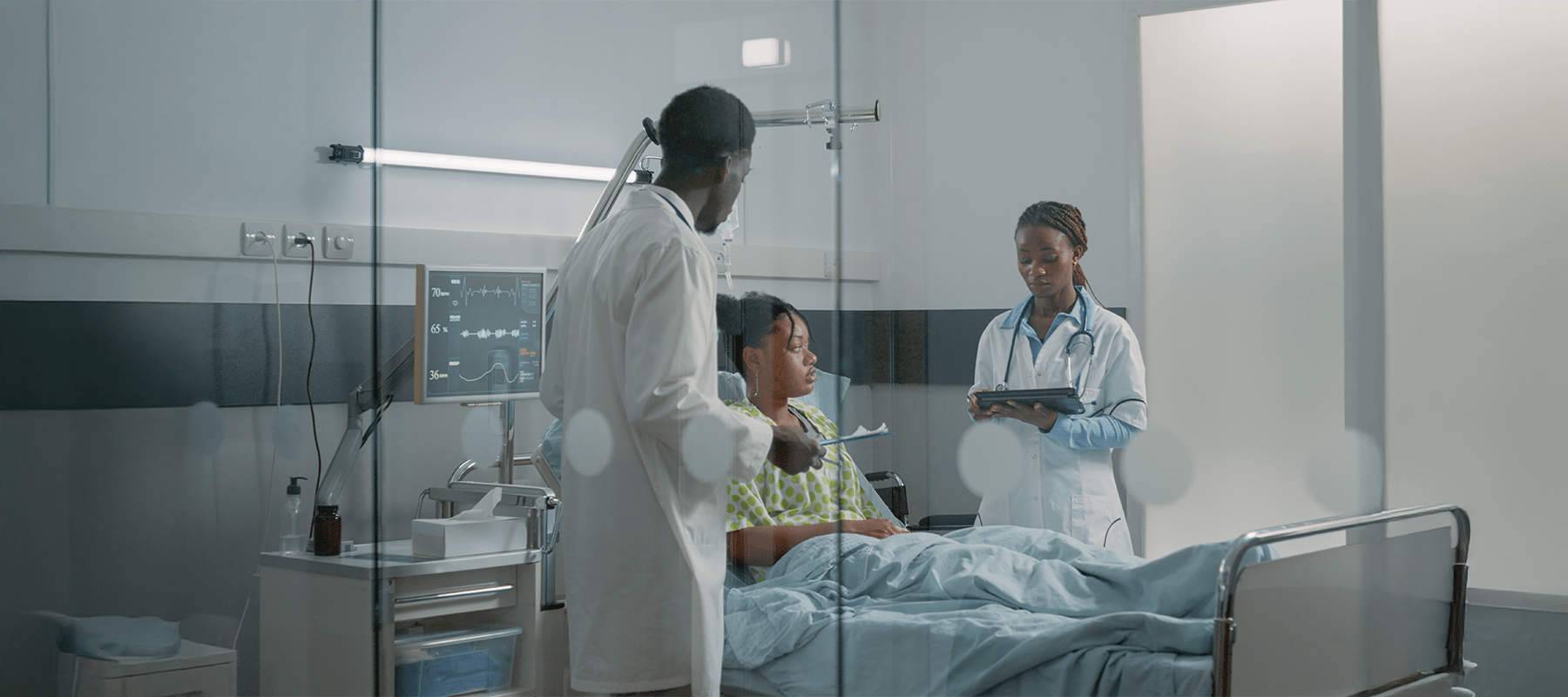
The role played by the mobile clinic revolution
Mobile clinic solutions for rural healthcare enter as the glimmer of hope to fill the void where ERs had once served the people. At these units, the patients receive flexible, lower-cost and community-based care. The mobile clinic benefits in rural areas cover rapid deployment, preventive services and often urgent interventions. Above all, the solutions have not been designed to replace hospitals entirely, but rather to serve as a lifeline.
How do mobile clinic solutions bridge the gap?
It is acceptable if you wonder how mobile clinics replace ER services in reality. Even if the setup cannot perform trauma surgery, the team can handle screenings, urgent care, vaccinations and chronic disease management. Thus, the distant hospitals are relieved of the strain, and it builds trust in vulnerable communities. The mobile clinic benefits in rural areas are tangible – people are assured of earlier diagnoses, less need to travel and continuity of care.
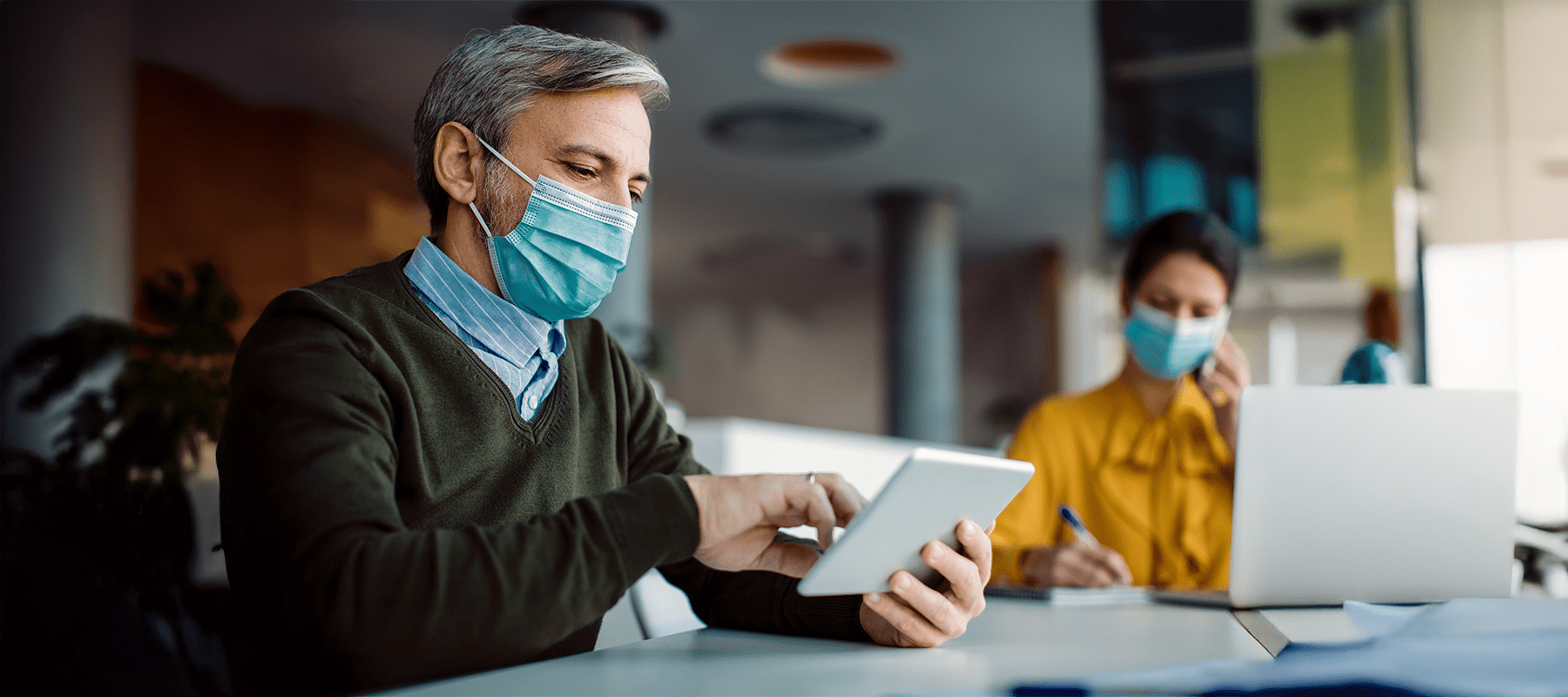
How does telemedicine help?
Rural telemedicine vs emergency care is another hot topic. While virtual consults scarcely substitute for a defibrillator or a surgical team, they are nevertheless able to stabilize patients, triage emergencies, and connect residents with specialists miles away. Telepath, being combined with mobile units, is proving to be a vital bridge – it might not be a complete solution.
Success stories from the field
Our theory is backed by proof. Successful mobile healthcare programs in the USA demonstrate the power of innovation in saving lives. From Texas to Kentucky, there has been a significant improvement on a vast scale. Programs are deploying vans, buses and pop-up clinics to improve preventive care rates. Thus, ER visits have reduced, and costs have come down. These mobile clinic benefits in rural areas are the representation of hope in action, particularly when funding and partnerships are in alignment.
Community resilience and adaptation
Regardless of the challenges, the rural residents are resilient. For legislative reforms, the communities are organizing ride-share networks, hosting health fairs and lobbying. Through these efforts, it is clear how determination can counter the effects of rural ER closures on patients. Often, grassroots energy fuels partnerships with non-profits and state health departments.
Role of Policy in Prevention
A stronger policy has to step in compulsorily. To reverse the rural healthcare crisis explained here, the crucial requirements include subsidies, better insurance reimbursement and incentives for staff recruitment. Taking responsibility, Federal intervention could delay the tide of rural hospital closures. On the other hand, it could encourage investment in mobile clinic solutions for rural healthcare.
A long-term outlook
The connection between rural hospital closures and mortality rates will continue to deepen if trends are allowed to continue unchecked. Small towns will encounter worsening healthcare disparities in rural communities. However, with innovation, advocacy and federal support, the rural healthcare crisis explained is capable of transforming itself into a success story of adaptation and resilience.
Reinventing small-town hospitals
Rural hospitals are likely to survive in reinvention. Starting from hybrid models combining urgent care with outpatient services and extending to partnerships with universities and non-profits, the hospitals have begun to explore ways to stay viable. With this rethinking, the rural health landscape can be reshaped, and the challenges of rural elderly healthcare challenges after ER closures can be alleviated.
Lessons for urban America
On an interesting note, even the city hospitals are studying how mobile clinics replace ER services. The lessons from successful mobile healthcare programs in the USA apply everywhere – what matters most are flexibility, prevention and community trust. Rural innovation could ultimately guide urban systems in reducing overcrowded ERs and improving patient outcomes.
On the whole,
The rural healthcare crisis explained is among America’s most urgent but least visible challenges. Because of rural hospital closures, the entire communities are becoming vulnerable, mortality is rising, and inequalities are deepening. Nevertheless, through mobile clinic solutions for rural healthcare, telemedicine, and community resilience, hope persists. The present-day actions define the future of healthcare equity – to ensure that no small towns face a medical emergency without a lifeline.

Rayan works closely with Eastpoint Digital, a reputed content marketing agency in California. He is dynamic in promoting and publishing blogs across various sites, focusing on generating quality backlinks to boost online visibility.