Bringing into the limelight: the vow undergoing a negligence phase… The U.S. government had made a promise to provide adequate Native American healthcare support as per the treaty and trust responsibility. However, this promise now stands among the topmost nations’ most profound failures. Because this chronic ongoing crisis is fundamentally rooted in the severe chronic underfunding of the Indian Health Service, Federal policy is being massively neglected and showcasing a lot of American health disparities. Thus, the Indigenous health outcomes are being devastated.
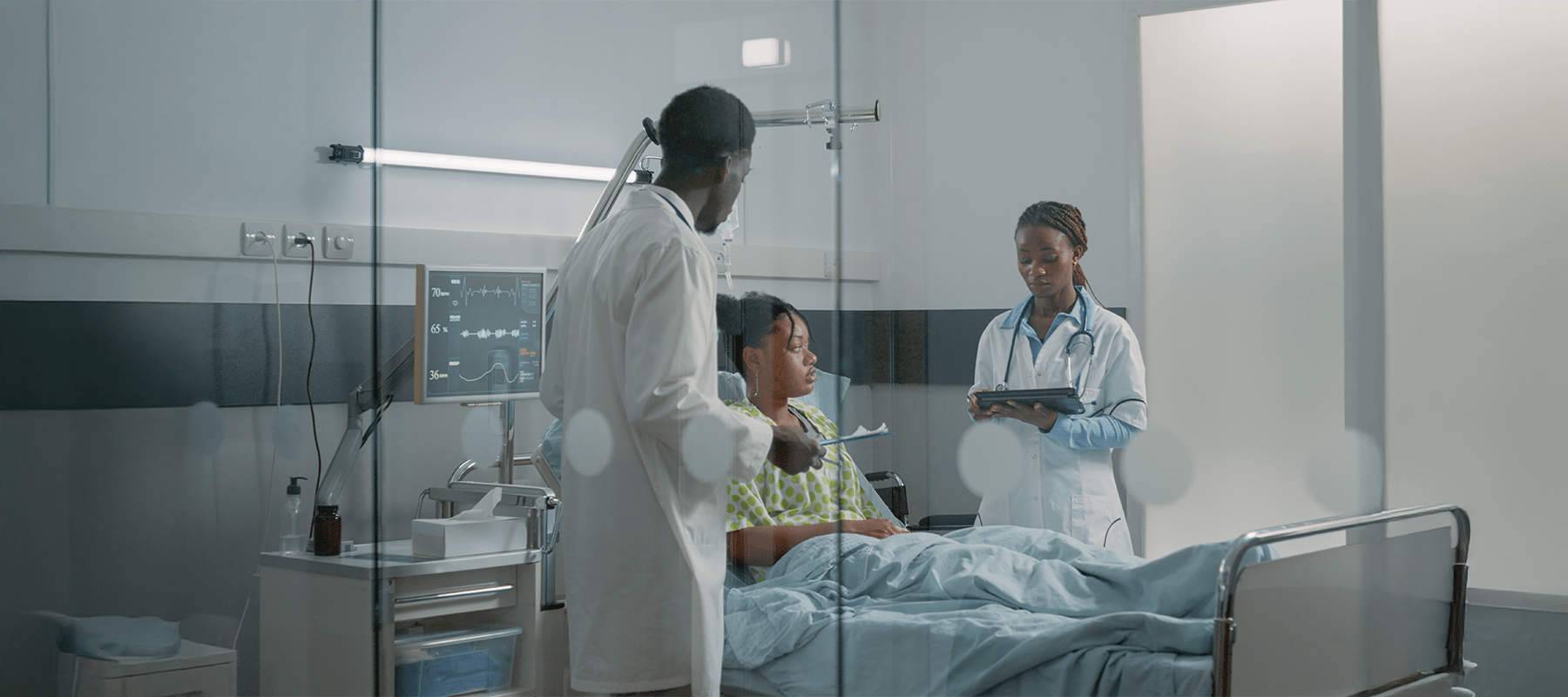
Spending formative years working with the Indian Health Service (IHS) and later with the tribal health systems, a healthcare professional has even witnessed this crisis firsthand. No doubt it is more than a policy failure – it concerns life and death, which highlights the severe inequities in Native American public health infrastructure. However, the healthcare professional took the vow to champion community-driven healthcare solutions in Native communities. Improving the IHS budget and tribal health autonomy should be the priority.
Coming to the chronic underfunding’s shadow:
How are the IHS budget gaps affecting the Native American Health outcomes?
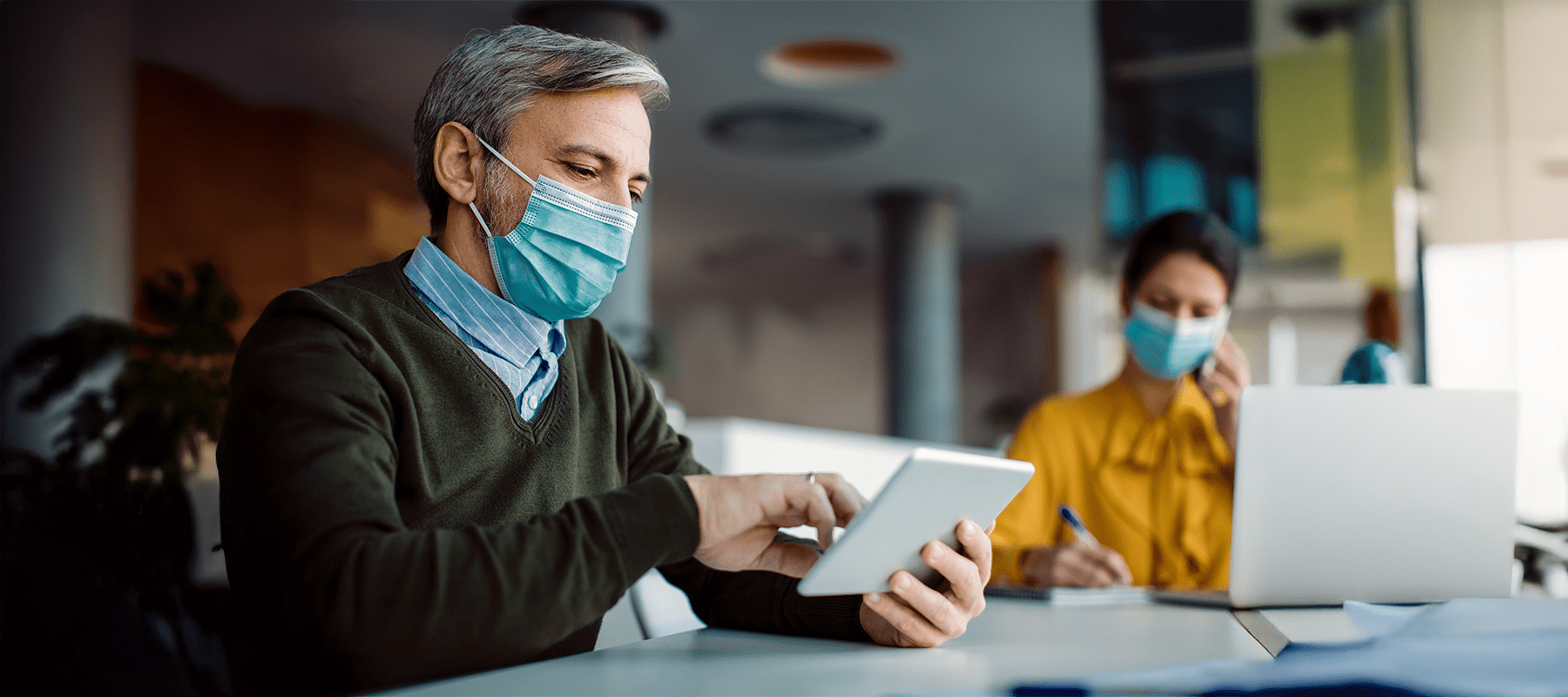
The IHS funding crisis is the core issue. Historically, what is needed for mission fulfillment – the Indian Health Service has received just a fraction of it. Now this severe chronic underfunding of the Indian Health Service indicates the per-capita spending on Native American healthcare is dramatically lower compared to the federal inmates, veterans, or the general public. Due to this persistent IHS funding crisis, the effects have been manifested in catastrophic ways that include dilapidated facilities, outdated equipment, and astronomical staff vacancy rates.
Because of this scarcity of access, the result is appalling Native American health disparities and federal policy failures. Ultimately, the scenario worsens the Indigenous health outcomes that disproportionately have high rates of heart diseases, diabetes, and preventable deaths. For these severe inequities in Native American public health infrastructure, the nation is facing a national shame. The current demand is immediate action for better Indigenous health support. Hence, it is all so clear how necessary it is to initiate improving the IHS budget and tribal health autonomy.

Talking about the policy puzzle:
Why is Native American healthcare still underfunded, and what are the reforms that could address the IHS budget gaps?
Discretionary funding status is the root cause of the IHS funding crisis. It is in dire need of annual congressional battles. Because of this instability, competitive salaries and infrastructure upgrades are at stake. As a result, it perpetuates the chronic underfunding of the Indian Health Service.
However, this issue can be solved by diverting the focus of policy reforms to concentrate the IHD budget on mandatory, advance appropriations, to ensure reliable federal responsibility for Native healthcare funding. Furthermore, to achieve genuine funding, the IHS budget is matched to the true cost of providing quality care while tackling the systemic inequities in Native American public health infrastructure with efficiency.
Accepting the tribal-led healthcare reforms in the United States and guaranteeing federal responsibility for Native healthcare funding is crucial to address the IHS funding crisis while securing future Native American healthcare access. This is the only way to seriously discuss improving the IHS budget and tribal health autonomy.
How can sovereignty bring in redemption?
What helps is community-driven healthcare innovations in native communities.
The IHS funding crisis might continue. However, the true redemption can be scaled in tribal-led healthcare reforms in the United States. Pioneering the community-driven healthcare solutions in the Native communities rewrites the success story. Collaborating with a Tribal Council becomes mandatory to address the lack of frustration to mental health resources and the resulting prescription of antidepressants for loneliness. It is one of the symptoms of underlying Native American health disparities and federal policy neglect. A culturally-relevant “Circle of Care” initiative has been launched to combat isolation and restore indigenous health. It is a model of grassroots healthcare initiatives in tribal regions.
Several tribal members were trained as “Social Prescribing Navigators,” which connected the elders to traditional healing and cultural activities. Setting this example of community-driven healthcare solutions in Native communities helped to demonstrate the power of tribal healthcare leadership. The successful grassroots healthcare initiatives in tribal regions significantly reduced unnecessary prescriptions. Thus, what has been proven is that tribal-led healthcare reforms in the United States are proven to be profoundly effective at addressing the Native American health disparities and federal policy as created by the chronic underfunding of the Indian Health Service.

Looking into a two-system reality:
Comparing Federal and Tribal healthcare systems for the Native American populations
Two systems complete the landscape of Native American healthcare. First, the Federal system or the Indian Health Service seems to have been crippled by the IHS funding crisis as well as the lack of Federal responsibility for Native healthcare funding. Second, the Tribal system covers the programs operated by the tribes under self-governance. These tribal healthcare systems, even if they are still relying on federal dollars, are consistently demonstrating superior outcomes by aligning care with cultural needs. As proven by this model, the tribal-led healthcare reforms in the United States stand out as the superior path.
The government has to uphold its federal responsibility for Native healthcare funding by providing stable, mandatory resources. It is the way to dismantle the pervasive inequities in Native American public health infrastructure. With this shift, the tribal healthcare systems have been empowered, which further supports the powerful grassroots healthcare initiatives in tribal regions, drifting apart from the failures of the Indian Health Service while heading toward real improvements in the IHS budget and tribal health autonomy.
Finally, a call for funding equity and action
Reaching the end of our discussion, it’s safe to include that the continuing IHS funding crisis is a moral and policy failure that is severely impacting Indigenous health and heightening Native American health disparities and federal policy inadequacies. Now Congress has to take over to fully embrace Federal responsibility for Native healthcare funding and provide true funding parity.
The clearest path to healing, as confirmed by the success of community-driven healthcare solutions in Native communities and numerous grassroots healthcare initiatives in tribal regions, confirms the empowerment of tribal healthcare leadership. Now we have to take steps to end the chronic underfunding of the Indian Health Service. We have to be prompt to address the severe inequities in Native American public health infrastructure while fully supporting improving the IHS budget and tribal health autonomy by means of robust tribal-led healthcare reforms in the United States
Pooja Saha is a passionate content writer who creates engaging, easy-to-understand, and SEO-friendly content. She specialises in crafting blogs and articles that connect with readers while helping brands grow online.